In This Article
Fibula fracture can happen easier than you’d imagine, usually with a simple rolled ankle. But this kind of broken bone doesn’t behave like you’d expect.
You can often walk on the ankle, despite pain when the fibula is broken. And it feels about the same as a bad break, so then level of pain doesn’t seem out of the ordinary.
Almost instantly, the fibula fracture will swell and bruise…much like a bad sprain. It hurts to move and when you stand on it, identical to a bad ankle sprain.
So how can you tell if you’ve broken your fibula, without waiting in an emergency department for an X-ray?
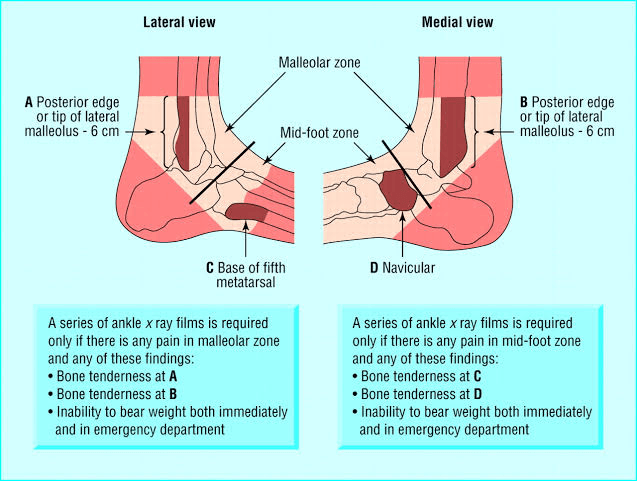
This is the exact situation that the Ottawa Ankles Rules were developed for. The Ottawa Ankle Rules are a great tool for anyone to identify the likelihood of a fracture after an ankle sprain. They actually cover 4 common fracture locations around the ankle – Fibula, Tibia, Navicular and 5th Metatarsal fractures.
The Ottawa Ankle Rules
The Ottawa Ankle Rules were designed to be used by junior medical staff in hospital Emergency Departments to screen for fractures. They don’t “diagnose” the fracture on their own, they just tell the clinician if an X-ray is needed.
They’ve been tested in large studies which found that:
- they’re as effective for experienced staff as they are for novice staff – you don’t need to be a highly-trained doctor to use them
- they’re really good at picking up fractures in these locations – they almost never miss one
- they sometimes highlight an issue when there is no fracture – there’s the occasional false alarm when there’s no fracture
So overall, anyone can use these tests and they’re great at telling you if you need an X-ray or not.
If they’re positive, getting a plain X-ray is usually good enough to confirm a fibula fracture. Some partial fractures (often called “greenstick fractures” in children, referring to the action of bending a green/fresh stick from a tree that bends and only partially cracks) may need a CT or MRI scan to diagnose if they don’t show up on X-ray, but that decision is best advised by the medical staff.
What can you do for a Fibula Fracture?
You can still walk with a fibula fracture! It’s a non-weight bearing bone, so you can still put weight through it (although it will be painful). The problem is that every time the ankle bends forward (known as dorsiflexion), it pushes on and moves the fracture.
You can stop the ankle bending with a camwalker boot, also known as a medical boot or moon boot. It’s a rigid boot that is worn every time you’re on your feet and is usually needs for 4-6 weeks. After 6 weeks of normal healing, the bone has 95% of its original strength back.
Wearing a boot can be clunky and uncomfortable but the alternative is a pair of crutches to take the weight off the foot, so you’ll be uncomfortable either way.
For the camwalker boot, you need a tall boot (also known as a 17″ boot) as it provides the best restriction to ankle movement. There are also other options like closed/protected toes, rigid tongues and inflatable bladders around the ankle.

Want help choosing the right cam walker boot?
Our Physio experts have listed the key features to look for when buying a cam walker boot (aka. medical boot or moon boot).
The recommendations make it simple to get the right boot first time, to speed up your recovery.
You can still walk around and exercise with a camwalker boot, although you’ll probably want to wait a week or two as the increased blod flow to the area can cause pain in a fresh fracture.
If you’d like some suggestions for exercise programs while you’re in a boot, our Physio team put together this awesome little program for home strength exercises.
Do you need surgery?
The simple answer is that surgery isn’t common for fibula fractures but some less common fracture types will required it.
If your fracture leaves the bone in its natural position and it’s a clean fracture line, wearing a boot for 4-6 weeks is usually enough to stabilise it while it heals.
Fractures that are displaced (shifted from their normal position) are more likely to require surgery to realign the fracture back to its natural position.
Comminuted (fragmented) fractures will also be considered for surgery as the chance of healing is improved if the fragments can be stabilised.
Open fractures (when the bone pierces the skin) will definitely get surgery to clean out the wound and protect the area from infection.
The normal surgical approach is referred to a “Open Reduction Internal Fixation”, abbreviated in medical notes to an “ORIF”. Open refers to opening up the area (ie. surgical incision), Reduction is the process of relocating the fracture, and Internal Fixation is using a medical device to hold the bone in place.
ORIF ranges from the most common approach of a plate screwed into the bone sections to the less common approach of a metal wire woven through the smaller comminuted fragments. That decision is based on the X-ray appearance and how it looks when they open the skin and see the fracture. You don’t need to worry about that part – surgeons generally know what they’re doing and will consider a range of factors when making the final decision.
What if the Ottawa Rules are all clear?
If Ottawa tests are negative/clear, you need to consider other possibilities for your injury.
By far, the most common injury after rolling an ankle (with very similar presentation to a fibula fracture) is a Lateral ankle sprain.
There are a number of less common diagnoses worth considering. If the pain came on gradually, it could be a Peroneal tendinopathy. If the pain is more central at the front of the ankle, it could be a Syndesmosis injury. If there is no tenderness to push on the posterior (back) of the fibula bone, it could be a Bone oedema/bruise.
